Managing Functional Constipation
A Pediatric Guide
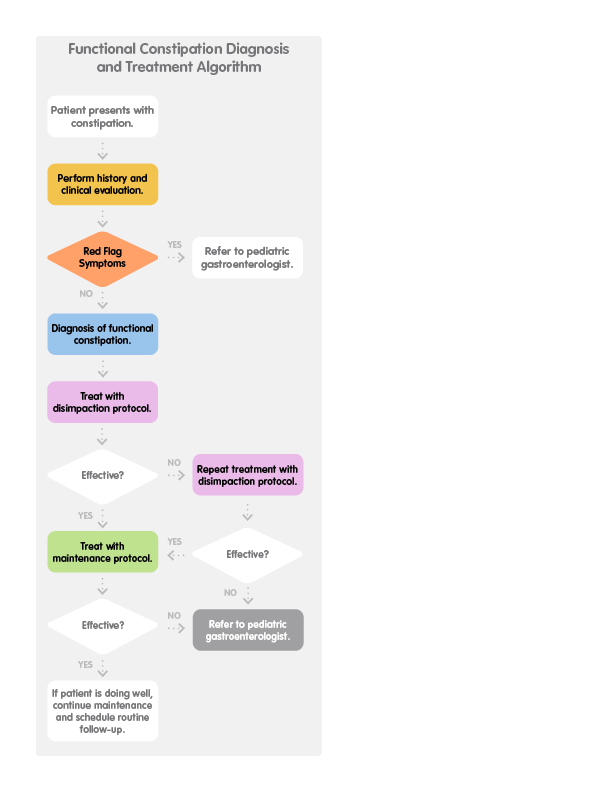
Constipation is an extremely common presenting symptom in children. To assist with patient diagnosis and treatment, the Children’s Mercy Gastroenterology team created the following recommendations.
Download a PDF of this full pediatric guide
DISCLAIMER: This content gives you general information about the described health conditions. This information does not take the place of a healthcare provider's training, experience, or judgment. You should not rely on this information in place of the advice of a healthcare provider. NO WARRANTY WHATSOEVER, WHETHER EXPRESS OR IMPLIED BY LAW, IS MADE WITH RESPECT TO THE CONTENT.
1. History and clinical evaluation
Functional constipation is defined by Rome IV criteria (consensus, expert, clinical definition based on symptoms only) and having at least 2 of the following for at least one month:
Infants to 4 years of age
- Two or fewer defecations per week.
- History of excessive stool retention.
- History of painful or hard bowel movements.
- History of large diameter stools.
- Presence of a large fecal mass in the rectum.
And in toilet trained children
- Soiling at least once a week with small or large amount of poop in underwear.
- History of large diameter stools which clog the toilet.
Children >4 years of age
- Two or fewer defecations per week in a child of developmental age at least 4 years.
- At least one episode of fecal incontinence per week.
- History of retentive posturing or excessive volitional stool retention.
- History of painful or hard bowel movements.
- Presence of a large fecal mass in the rectum.
- History of large diameter stools which can obstruct the toilet.
Symptoms cannot be explained by another condition.
2. Red flag symptoms*
Though constipation is prevalent in children and infrequently a result of underlying intestinal or systemic disease, red flag symptoms and diagnostic clues should be used to identify an underlying disease responsible for constipation. If the patient displays one or more of the red flag symptoms below, referral to pediatric gastroenterology is indicated.
- Delayed passage of meconium (>48 hours in a term newborn)
- Failure to thrive
- Bloody stools
- Severe abdominal distention
- Perianal fistula
- Absent anal wink
- Sacral dimple
*See Consensus Guidelines from North American Society for Pediatric Gastroenterology, Hepatology and Nutrition for additional guidance.
3. Diagnosis
In the absence of clinical features indicative of a specific disorder, or red flag symptoms, testing is not recommended or required to make the diagnosis of functional constipation. Abdominal X-ray is NOT recommended unless a bowel obstruction is suspected. When possible, the diagnosis of functional constipation should be based on clinical history and physical exam.
4. Treatment
Pro tips to offer parents: How to take Miralax daily for cleanout
- Mix and let sit for 10 minutes before serving.
- Try a variety of clear liquids.
- Serve with a straw.
- Serve at different temperatures to see what the child likes best.
- Offer a reward for completion.
Frequently used maintenance medical management includes dietary modification or use of osmotic laxatives. Although sometimes effective, dietary modification for pediatric functional constipation has poor evidence to support its use.
General treatment of constipation:
- Identification of constipation as the diagnosis.
- Education of the patient and family about the diagnosis.
- Expectations for treatment (often protracted, requires a routine).
- Goals for treatment (soft bowel movements that are easy to get out, achieve continence).
- Cleanout/disimpaction if large stool burden is present.
- Maintenance medical and behavioral management plan to prevent exacerbation.
Medical therapy and dosage recommendations for disimpaction*
- Oral (preferred)
- Polyethylene glycol solution 1–1.5 g/kg/day x 3–6 consecutive days
- Magnesium citrate 4 mL/kg/day x 2 consecutive days
- Rectal
- Normal saline enema 10 mL/kg x 3 consecutive days
- Sodium phosphate enema x 3 consecutive days
- 2–4 years: one-half contents of a 2.25-oz pediatric enema
- 5–11 years: 2.25-oz pediatric enema
- >12 years: 4.5-oz enema
- Mineral oil enema x 3 consecutive days
- 2–11 years: one-half contents of a 4.5-oz bottle
- >12 years: 4.5-oz bottle
- Nasogastric (requires hospital admission)
- Polyethylene glycol solution 25–40 mL/kg/hr until rectal effluent is clear (24–48 hr)
- Polyethylene glycol solution 25–40 mL/kg/hr until rectal effluent is clear (24–48 hr)
- For school-aged children, start protocol on a Friday night.
- If results are satisfactory, provide parents with Maintenance Therapy Protocol.
- If results are unsatisfactory, repeat disimpaction protocol.
- If results are still unsatisfactory, consider referral.
Maintenance therapy and dosage recommendations for chronic constipation*
- Osmotic laxatives
- Polyethylene glycol 1 g/kg/day
- Lactulose 1–3 mL/kg/day divided into 2 doses
- Magnesium hydroxide
- <2 years: 0.5 mg/kg/dose
- 2–5 years: 5–15 mg/day once before bedtime or in divided doses
- 6–11 years: 15–30 mg/day once before bedtime or in divided doses
- >12 years: 30–60 mg/day once before bedtime or in divided doses
- Stool softeners/lubricants
- Mineral oil 1–3 mL/kg/day divided into 2 doses
- Stimulant laxatives (can also be used for rescue therapy)
- Senna
- 1 month–2 years: 2.2–4.4 mg/day at bedtime or in 2 divided doses
- 2–6 years: 4.4–6.6 mg/day at bedtime or in 2 divided doses
- 6–12 years: 8.8–13.2 mg/day at bedtime or in 2 divided doses
- >12 years: 17.6–26.4 mg/day at bedtime or in 2 divided doses
- Bisacodyl
- 3–12 years: 5–10 mg/day
- >12 years: 5–15 mg/day
- Senna
- If results are unsatisfactory for maintenance protocol, instruct parents to contact physician for follow-up evaluation.
- If patient is doing well, continue maintenance and schedule routine follow-up.
*Disimpaction and Maintenance Therapy Protocols from: Constipation and Encopresis in Childhood. Pediatrics in Review. Published Sept. 30, 2015. Jennifer M. Colombo, MD, Matthew C. Wassom, PhD, John M. Rosen, MD. Division of Gastroenterology, Children’s Mercy, University of Missouri-Kansas City School of Medicine, Kansas City, MO.
5. Referral instructions
Children who do not respond to the disimpaction or maintenance therapies may require a referral to a pediatric gastroenterologist for further evaluation.
The BRICK (Bowel Retraining in Constipated Kids) Clinic is a special clinic within the Division of Gastroenterology at Children’s Mercy. It was developed to provide children with severe, chronic constipation a comprehensive program to improve their bowel function.
This clinic cares for children 3 years and older who are otherwise healthy, but who have symptoms that include, but are not limited to encopresis, constipation, large or hard stools, infrequent stools and/or stool withholding.
Make a referral
Select “GI General Clinic” from the list of specialties and “Constipation (BRICK Clinic)” under “Reasons for Consultation.” Note: Patients who do not meet the criteria for the BRICK Clinic can be referred to the “GI General Clinic.” Follow the same steps, but select the most appropriate reason for consultation, then complete the remaining fields and submit.
All new referral requests are processed within 48 hours. Two phone attempts to contact the family and a final notification to the family to schedule will be made. For assistance, call the Contact Center at (816) 234-3700 or toll-free at (800) 800-7300. The Contact Center can provide additional information regarding any supporting documentation needed for the referral.
For urgent requests to speak to a specialist, please call and ask to speak with the on-call pediatric subspecialist at 1 (800) GO-MERCY / (800) 466-3729.
These instructions are provided for informational purposes only. The choice of provider referral is at your discretion.
What to tell families
Education is as important as medical therapy in successfully managing functional constipation.
- Give parents written home management instructions, either as a print-out or via email following their visit.
- Recognize withholding behaviors and use behavioral interventions:
- Regular toileting. Tell parents that the child is to sit on toilet 2 to 3 times daily, 5 to 10 minutes each, for “protected time to have a BM.” Ensure that smaller children have a step stool so feet touch solid surface.
- Use diaries to track stooling.
- Emphasize positive reinforcement, not punishment.
- Recommend normal fiber and fluid intake for age. Addition of prebiotics and probiotics to the regimen is not currently supported by adequate evidence.
- Set definitive follow-up appointment within several weeks to assess progress and provide additional guidance. Encourage follow-up phone calls to remain on track.
- Emphasize if families are having difficulties, they should follow up to discuss referral to a pediatric gastroenterologist.
Children’s Mercy has created resources for families on the topics of functional constipation and encopresis. Read “Unstuck: Your Family’s Guide to Childhood Constipation.”