Clubfoot Deformity in Children: Modern Treatment for the World
State of the Art Pediatrics - January 2023
Column Author: Richard M. Schwend, MD, FAAP, FAOA | Pediatric Orthopedic Surgery; Rex L Diveley Endowed Professorship in Orthopedic Research; Interim Chair Department of Orthopedic Surgery; Director, Pediatric Orthopedic Surgery Research Program; Past Chair, American Academy of Pediatrics, Section on Orthopedics; Past President, Pediatric Orthopedic Society North America; Professor of Orthopedic Surgery, University of Missouri-Kansas City School of Medicine; Clinical Professor of Orthopedic Surgery, University of Kansas School of Medicine
Column Editor: Amita Amonker, MD, FAAP | Pediatrics; Pediatric Hospitalist; Assistant Professor of Pediatrics, University of Missouri-Kansas City School of Medicine; Clinical Assistant Professor of Pediatrics, University of Kansas School of Medicine
Background
Congenital idiopathic clubfoot is the most common serious musculoskeletal birth defect worldwide. Without treatment the condition typically becomes a lifelong disability affecting quality of life and function. Idiopathic clubfoot occurs in an otherwise normal infant and is a separate entity from syndromic or neuromuscular associated clubfoot. Idiopathic clubfoot is more common, easier to treat, and has less chance of recurrence during and after treatment.
In the United States, about 1 in 1,000 infants is born with an idiopathic clubfoot. There is a 2:1 ratio of male:female, and 40% of cases are bilateral. A true idiopathic clubfoot is quite stiff and should not be confused with the more common foot deformity that results from intrauterine crowding, which is flexible and often self-correcting. Idiopathic clubfoot is typically an isolated congenital abnormality, secondary to multifactorial environmental and genetics factors, with a 35% concordance in identical twins.
A clubfoot may be discovered during routine prenatal ultrasonography. When a clubfoot is detected, a thorough ultrasound examination is required to detect additional findings to exclude syndromic or neurogenic cause. When a clubfoot is detected prenatally, fetal MRI has been suggested to reliably assess for other associated findings. Pediatric orthopedic surgeons are frequently asked to offer prenatal counseling to the parents to prepare them in advance for the diagnosis and eventual treatment. Prenatal counseling can greatly help with parental anxiety about this diagnosis. The false positive rate of clubfoot deformity has been estimated at 19%, so not all clubfeet suspected prenatally are true clubfeet when the child is born. This possibility should be discussed in advance with the parents.
At birth, a thorough general examination is performed to evaluate for common syndromes and neurological conditions such as spina bifida, lipomeningocele, tethered spinal cord, sacral agenesis, arthrogryposis or limb deficiencies. A true clubfoot will have a thinner calf, and the foot may have medial and posterior creases. A positional foot deformity can be easily corrected beyond normal. The clubfoot deformity has four key components best remembered by the acronym “CAVE”: The midfoot has a high arch (cavus), the forefoot is pointed inward (adductus), the heel is inverted (varus), and the heel is pointed in plantarflexion (equinus). (Figure) Radiographs are generally not necessary. A geneticist can assist in the evaluation when there is concern for a syndrome.
Without treatment the foot will persist with the clubfoot deformity. The child will begin walking on the lateral side or even dorsum of the foot, although walking age is not typically delayed. Older children and adults may have difficulty wearing standard shoes. Especially in countries with limited resources, the physical and social limitations can affect a person’s options for education or employment and can be a barrier to marriage or a normal social life.
Treatment
The Ponseti method of clubfoot management has become the standard of care worldwide. Prior to the general acceptance of the Ponseti technique, pediatric orthopedic surgeons had been frustrated by the long-term outcomes of traditional clubfoot treatment. Previous extensive surgical and nonsurgical treatments or combinations of the two often looked promising in the short term, only to be followed by recurrent deformity with pain and stiffness as the child reached skeletal maturity and beyond into adulthood.
The Ponseti method is named for lgnacio Ponseti, MD (1914-2009), who became a professor of orthopedic surgery at the University of Iowa after immigrating from Spain. In 1948 Dr. Ponseti developed his method of conservative treatment based on a clear understanding of the patho-anatomy of the clubfoot and how it affects foot biomechanics. One of the important distinctions of his method was a series of weekly casting followed by a prolonged bracing phase that lessened but did not eliminate recurrences of the deformity.
Phase 1: The first phase is a specific casting technique that ideally should start soon after the baby leaves the newborn nursery, at about 1-3 weeks of age. However, there are reports of successful initiation of casting even when initiated at several years of age. The long leg casts are changed weekly until most of the deformity is corrected.
Phase 2: A percutaneous Achilles tenotomy done under local lidocaine anesthesia in the clinic is required for about 90% of cases and is followed by a final long leg cast for three weeks. Because the tenotomy is so frequently required as part of the Ponseti method, it is important to counsel the family that this is still a surgical procedure, rather than being completely non-operative. However, it is standard to do the procedure in the clinic, given concerns about anesthesia and neurotoxicity at this young age.
Phase 3: Following the period of casting is a prolonged period of bracing full time (23 hours/day) for three months, and then nighttime/naptime only (12-14 hours/day) until the child is 4 to 5 years old. The brace is a bar with shoes attached at shoulder width. The shoe is turned out 60-70 degrees on the clubfoot side and 30-40 degrees on the normal side.
Phases 1 and 2 should be performed by a physician experienced with the technique, typically a pediatric orthopedic surgeon. If no local physician is experienced with the Ponseti technique, the family should travel for care. Phase 3 is most important, because without prolonged nighttime/naptime bracing until age 4 to 5 years, the clubfoot deformity will most likely recur.
Communication and Teamwork for Best Results
It is not easy for a family to keep a child in a brace every night for four years, especially when the foot looks and functions normally. Fortunately, significant improvements in brace design have made them much easier for parents to apply and for children to tolerate. The old stiff shoes that were rigidly fixed to the bar have been replaced by detachable shoes or splints with soft linings. The child’s pediatrician and pediatric orthopedic surgeon should work as a team in helping families comply with the bracing phase. Barriers to compliance should be explored and corrected. Adherence to bracing can be improved with culturally sensitive education, a positive communication approach, and family awareness of the importance of bracing. However, even with perfect compliance, the clubfoot deformity may recur. When this happens, casting is repeated, and bracing must be resumed.
With good compliance to brace wear, recurrence occurs in only about 6% of cases, but with poor compliance, recurrence occurs in up to 80%. In a small percentage of cases (5%-20%), the deformity recurs despite repeated casting and bracing. When this happens, the anterior tibial tendon can be transferred to the third cuneiform bone, which is part of the Ponseti technique. By following the method as originally described by Professor Ponseti, it should be extremely rare for a child to require the extensive joint release surgery that was standard before the year 2000. It is also important for parents to know that idiopathic clubfoot is an isolated finding, and that children who undergo Ponseti treatment and are successful with bracing can be expected to wear normal shoes, participate in sports, and have every opportunity for a happy and productive life.
Eighty percent of the over 200,000 babies born worldwide with clubfoot live in countries with limited resources where adults with untreated clubfoot face a life of poverty and isolation. The Ponseti method requires minimal resources and can be performed by non-physician health professionals who are taught the method by Ponseti experts. Programs have been started in many countries with limited resources with the goal of eliminating from the world the disability caused by untreated clubfoot.
Thanks to his genius and foresight, Dr. Ponseti’s method has become the standard of care worldwide for children with clubfoot deformity.
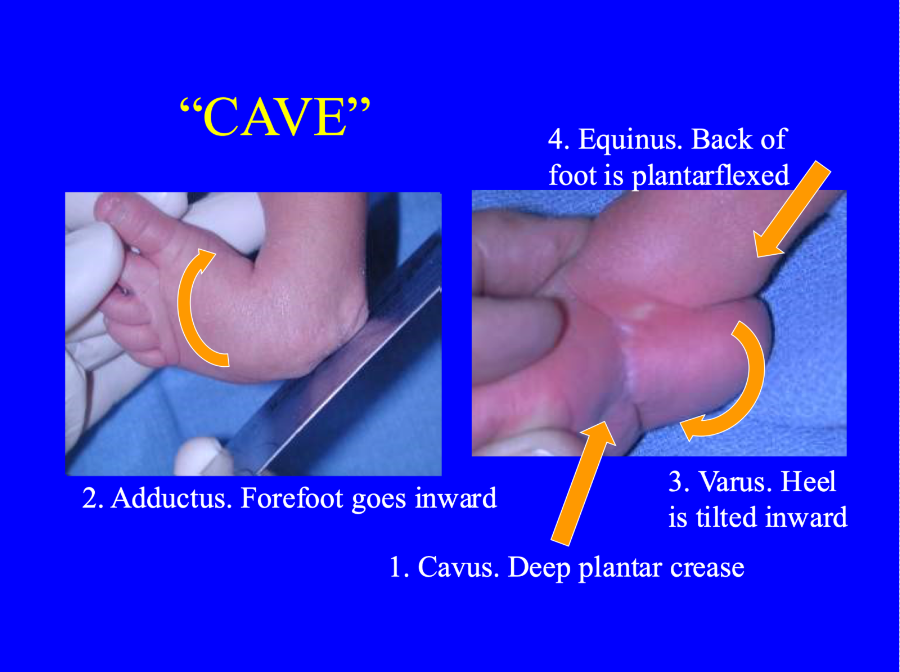
Figure. Clubfoot deformity can be remembered by the mnemonic “CAVE”: Cavus, Adductus, Varus and Equinus. The severity of a clubfoot can be graded by degree of deformity of these components.
Resources:
Cady R, Hennessey TA, Schwend RM. Diagnosis and treatment of idiopathic congenital clubfoot. Pediatrics. 2022;149(2):73-81. https://doi.org/10.1542/peds.2021-055555
See all the articles in this month's Link Newsletter
Stay up to date on the latest developments and innovations in pediatric care -- read the January issue of The Link.
